Wernicke’s encephalopathy is a devastating condition caused by a thiamine deficiency. Common symptoms of the disorder include confusion, ataxic gait, and oculomotor dysfunction. It may be difficult to diagnose in the beginning, but can be life-threatening if untreated. Here are the patients most at risk of developing WKS
 The disease is usually reversible with the correct treatment. Treatment for Wernicke’s encephalopathy is aimed at restoring function to the affected area. Acute thiamine deficiency is the primary cause of this neurodegenerative disorder. Clinical features of Wernicke’s encephalopathy include ataxia, altered mental status, and ocular dysfunction, though they rarely occur together. The important point to remember is that early detection of Wernicke’s encephalopathies is the key to preventing the clinical progression of the disease.
The disease is usually reversible with the correct treatment. Treatment for Wernicke’s encephalopathy is aimed at restoring function to the affected area. Acute thiamine deficiency is the primary cause of this neurodegenerative disorder. Clinical features of Wernicke’s encephalopathy include ataxia, altered mental status, and ocular dysfunction, though they rarely occur together. The important point to remember is that early detection of Wernicke’s encephalopathies is the key to preventing the clinical progression of the disease.
A 26-year-old woman presented to the department of surgery with persistent vomiting and nystagmus. Her symptoms were disruptive to her daily activities. Her doctor diagnosed Wernicke’s encephalopathy and prescribed a course of high-dose IV vitamin B1. The patient’s symptoms slowly improved.
Patients with Wernicke encephalopathy may experience acute mental confusion, ataxia, and ophthalmoplegia. Acute alcoholism and prolonged carbohydrate loading may also precipitate Wernicke encephalopathy. Patients with chronic alcohol abuse should be considered for further testing. Other symptoms of the disease include ataxia, hypotension, and delirium.
Wernicke’s encephalopathy is a serious condition that can lead to long-term hospitalization and death. The occurrence of Wernicke’s encephalopathy in children is increasing each year. Although the diagnosis is not fully understood, timely treatment with parenteral thiamine may help save the brain. It is inexpensive, safe, and has proven to be an effective treatment.
There is a high mortality rate associated with Wernicke’s encephalopathy, which ranges from 17 to 20 percent. In addition, approximately eighty-five percent of affected patients develop chronic memory deficits. In some patients, Korsakoff’s psychosis also develops.
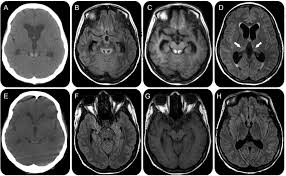
Neuroimaging scans can be helpful in determining the extent of neurological abnormalities in patients with WE. However, the specific areas of the brain affected by the disease vary widely between individuals. In approximately 58% of patients, there are ‘typical’ lesions in MRI scans. In addition, the cerebellum and mamillary body may be smaller than normal.
